Peri-Implant Surgery
[An Example of OralPedia.org entry]
Incisions and Flaps in Periodontal and Peri-Implant Surgery
Felipe Bravo, Bruna de C. F. Vajgel, Estela S. Gusmão and Renata Cimões
The principles of periodontal surgery, in general, do not differ from the surgical principles applied to other parts of the body. In order to perform a successful surgical procedure there are several important aspects to consider, namely: gentle tissue manipulation; firm and precise incisions; careful retraction of the flap; use of a traumatic suture techniques, and promotion of stable wound healing. Well-planned incisions are essential to gain access to the surgical site. When planning the incision, the main considerations must be the anatomy, surgical goal, and the design and a traumatic management of the flap. It is worth emphasizing the importance of a well-sharpened cutting instrument, in order to prevent unnecessary tissue damage. Clean and defined incisions will lead to better healing and less discomfort to the patient.
1 External Bevel
This is an incision contained in the gingiva and directed toward the crown of the tooth, with the object of eliminating pockets, improving gingival contour, and gaining access to the roots. This type of incision is frequently used in conjunction with flap surgeries when it is necessary to thin the tissue externally. It must be performed before folding the flap1. This incision is highly prevalent when performing gingivectomy surgeries [3-8].
1.1 Technique
The incision is contained in the gingiva and made in the direction toward the crown of the tooth. The instrument is placed at an angle of 45 degrees in the direction toward the pocket or gingival sulcus, or in relation to the root of the tooth. It may be linear or it may outline the gingival parabola (Figure 1). In the external bevel incision, the angle is 45 degrees in relation to the root.
2 Internal Bevel
This is a basic incision for the majority of flap procedures in periodontics, which is the primary incision when performing many flap procedures [1, 6]. The aim of this internal bevel decision is to remove the epithelium from the pocket to provide direct contact between the bone and healthy connective tissue [1]. Presently, this is done with three important objectives: to remove the pocket lining, to preserve the uninvolved external surface of the gingiva, and to produce a thin, fine gingival margin for bone-to-tooth adaptation [6]. This type of incision is also denominated the inverted or reverse bevel.
2.1 Technique
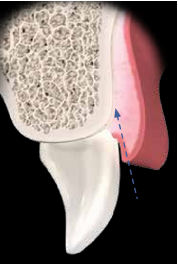
One begins at a certain distance from the gingival margin and ends at the bone crest; the inclination of the incision is inverse to the incision for gingivectomy, as it is made at an angle of 45 degrees in relation to the crown. The blade is placed parallel to the long axis of the tooth in the apical direction toward the alveolar crest, and is placed on the crest of the margin, or 0.5 to 2.0 mm away from it. The contour is dictated by the anatomy of the tooth and shape of the root (Figure 2).
Figure 2. Internal bevel incision showing the distance away from the gingival margin. The incision is angulated in the direction of the alveolar crest (A, B); front view of the internal bevel incision (C).
3 Sulcular Incision
This incision is performed when one wishes to preserve all the existent keratinized tissue [1]. It may also be denominated the secondary incision [6].
3.1 Technique
The scalpel blade is inserted into the gingival sulcus, parallel to the long axis of the tooth, in the direction toward the alveolar crest. This technique requires the inclusion of the largest possible amount of papillaein the flap (Figure 3).
Figure 3. Side view of an intrasulcular incision, showing that the incision is directed into the gingival sulcus (A, B); front view of the intrasulcular incision (C); intrasulcular incision in the palatal region (D).
4 Relaxing Incision
This type of incision may also be denominated the vertical or oblique relaxing incision. Relaxing incisions must extend beyond the mucogingival line in order to allow the flap to be displaced, and they should be avoided in the lingual and palatal areas [6]. They are made perpendicular to the gingival margin, increasing access to the alveolar bone, in addition to diminishing the tension of flaps. They also allow apical and coronal positioning of flaps, and limit the inclusion of a healthy site in the surgical field. Furthermore, relaxing incisions must not be made in pronounced concavities, must not divide the interdental papillae, and must not be located in the middle portion of the teeth (Figure 4).
Figure 4. Relaxing incisions. Incorrect location of the relaxing incision (A-C); correct location of the relaxing incision (D-F).
4.1 Technique
Incisions are made with the scalpel in the perpendicular position, and may or may not include the papillae in the flap. The incision must not cross the prominence of the adjacent tooth root (Figure 5).
Figure 5. Unilateral relaxing incisions (A, B); bilateral relaxing incision (C); positioning the scalpel blade to perform relaxing incisions (D).